Stemming from the post 'Blood Donation'; this post looks at the different blood groups that are present in human bodies and also some UK statistics. There are four different blood groups in the ABO blood system (A, B, AB and O (originally C)) which are each split into two groups via the Rhesus system where Rhesus is positive and without is negative i.e. A Rhesus (+) and A-.
A slice of history: "early attempts at blood transfusions, as far back as 1666, seemed to have been very successful, but when a French patient died unexpectedly during a procedure in 1668 all efforts were halted" (NHS Blood and Transplant: Blood Groups Leaflet).
But what segregates these different groups from each other? It is all down to the antigens (markers on the surface of red blood cells) and the antibodies (part of the specific immune response secreted by B effector cells to cluster 'foreign material' to be destroyed by macrophages) present in the blood. Between the blood types there are three types of antigens (A antigens, B antigens and Rhesus antigens) and two types of antigens (anti-A and anti-B).
A+ blood contains anti-B antibodies and red blood cells with A antigens and Rhesus antigens.
A- blood contains anti-B antibodies and red blood cells with A antigens but no Rhesus antigens.
B+ blood contains anti-A antibodies and red blood cells with B and Rhesus antigens.
B- blood contains anti-A antibodies and red blood cells with B but no Rhesus antigens.
AB+ blood contains no antibodies and red blood cells with A antigens, B antigens plus Rhesus antigens.
AB- blood contains no antibodies and red blood cells with A antigens, B antigens but no Rhesus antigens.
O+ blood contains anti-B and anti-A antibodies but red blood cells with no A or B antigens, just Rhesus antigens.
O- blood contains anti-B and anti-A antibodies with no antigens on the surface of the red blood cells.
These properties of the different blood groups are responsible for how they can be used and to whom they can be used by. If anti-A antibodies come into contact with A antigens they will attack the red blood cells and destroy them. This is the same reaction if anti-B antibodies come into contact with B antigens. If the blood groups are mixed then the results can be life threatening as we saw earlier with the French patient who died in 1668. This is because they did not know about the different blood groups, with the "ABO groups only discovered in 1901/1902 by Karl Landsteiner" (NHS Blood and Transplant: Blood Groups Leaflet) and the Rhesus groups discovered in 1937. Below is a bar chart of the percentages of each blood group present in the UK population with the most common being A+ and O+ and the rarest being AB-.
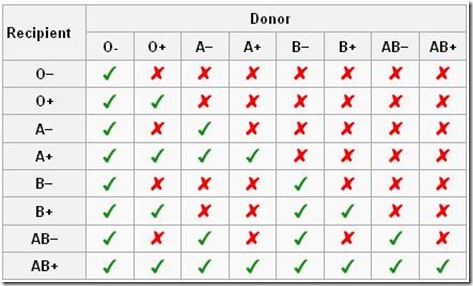
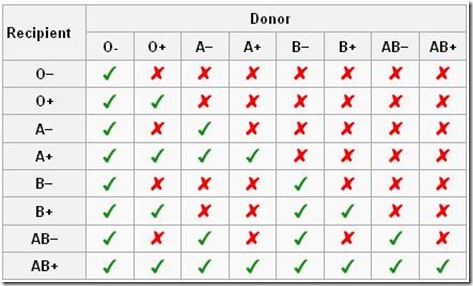
But what are the uses for each of the groups. Because of O- not having any antigens on its red blood cells it is known as the 'universal donor' as it can be given to anyone. This is because it cannot be targeted by any antibodies in the 'foreign' blood. At the other end: AB+ is the 'universal recipient' as a person with this blood group can receive any blood type due to having no anti-A or anti-B antibodies . However AB cannot be donated to people with either A or B blood types due to having both of these antigens on the surface of its red blood cells. Below is a table illustrating who can and can't receive each blood type. See if you can use the information provided above (about the antibodies and antigens with each blood group) to give reasons for why the recipient cannot receive certain blood groups.
Although in some cases it does not work like this and is known as the Bombay phenotype (http://anthro.palomar.edu/blood/Bombay_pheno.htm).
A slice of history: "early attempts at blood transfusions, as far back as 1666, seemed to have been very successful, but when a French patient died unexpectedly during a procedure in 1668 all efforts were halted" (NHS Blood and Transplant: Blood Groups Leaflet).
But what segregates these different groups from each other? It is all down to the antigens (markers on the surface of red blood cells) and the antibodies (part of the specific immune response secreted by B effector cells to cluster 'foreign material' to be destroyed by macrophages) present in the blood. Between the blood types there are three types of antigens (A antigens, B antigens and Rhesus antigens) and two types of antigens (anti-A and anti-B).
A+ blood contains anti-B antibodies and red blood cells with A antigens and Rhesus antigens.
A- blood contains anti-B antibodies and red blood cells with A antigens but no Rhesus antigens.
B+ blood contains anti-A antibodies and red blood cells with B and Rhesus antigens.
B- blood contains anti-A antibodies and red blood cells with B but no Rhesus antigens.
AB+ blood contains no antibodies and red blood cells with A antigens, B antigens plus Rhesus antigens.
AB- blood contains no antibodies and red blood cells with A antigens, B antigens but no Rhesus antigens.
O+ blood contains anti-B and anti-A antibodies but red blood cells with no A or B antigens, just Rhesus antigens.
O- blood contains anti-B and anti-A antibodies with no antigens on the surface of the red blood cells.
These properties of the different blood groups are responsible for how they can be used and to whom they can be used by. If anti-A antibodies come into contact with A antigens they will attack the red blood cells and destroy them. This is the same reaction if anti-B antibodies come into contact with B antigens. If the blood groups are mixed then the results can be life threatening as we saw earlier with the French patient who died in 1668. This is because they did not know about the different blood groups, with the "ABO groups only discovered in 1901/1902 by Karl Landsteiner" (NHS Blood and Transplant: Blood Groups Leaflet) and the Rhesus groups discovered in 1937. Below is a bar chart of the percentages of each blood group present in the UK population with the most common being A+ and O+ and the rarest being AB-.
But what are the uses for each of the groups. Because of O- not having any antigens on its red blood cells it is known as the 'universal donor' as it can be given to anyone. This is because it cannot be targeted by any antibodies in the 'foreign' blood. At the other end: AB+ is the 'universal recipient' as a person with this blood group can receive any blood type due to having no anti-A or anti-B antibodies . However AB cannot be donated to people with either A or B blood types due to having both of these antigens on the surface of its red blood cells. Below is a table illustrating who can and can't receive each blood type. See if you can use the information provided above (about the antibodies and antigens with each blood group) to give reasons for why the recipient cannot receive certain blood groups.
How do you become a certain blood type? "ABO blood types are inherited through genes on chromosome 9 and they do not change as a result of environmental influences during life" (http://anthro.palomar.edu/blood/ABO_system.htm). "A and B are co-dominant alleles over O thus if a genotype of one parent is AO then its genotype is A" (as above). The table below shows the possible outcomes:
| Parent Alleles | A | B | O |
|---|---|---|---|
| A | AA (A) | AB (AB) | AO (A) |
| B | AB (AB) | BB (B) | BO (B) |
| O | AO (A) | BO (B) | OO (O) |



